Non-Alcoholic Fatty Liver Disease (NAFLD) is a condition where excess fat builds up in the liver, not due to alcohol consumption. It affects roughly 25% of the global population, with higher rates among those with obesity and metabolic disorders[1]. Despite its growing prevalence, NAFLD often goes undiagnosed because it’s typically asymptomatic in its early stages, making it a silent but significant public health issue.
Table of Contents
- Definition and Spectrum
- Causes and Risk Factors
- Symptoms and Diagnosis
- Potential Complications
- NAFLD vs MASLD
- Treatment and Management
- Prevention Strategies
- FAQ
- References
Definition and Spectrum
NAFLD includes two major subtypes:
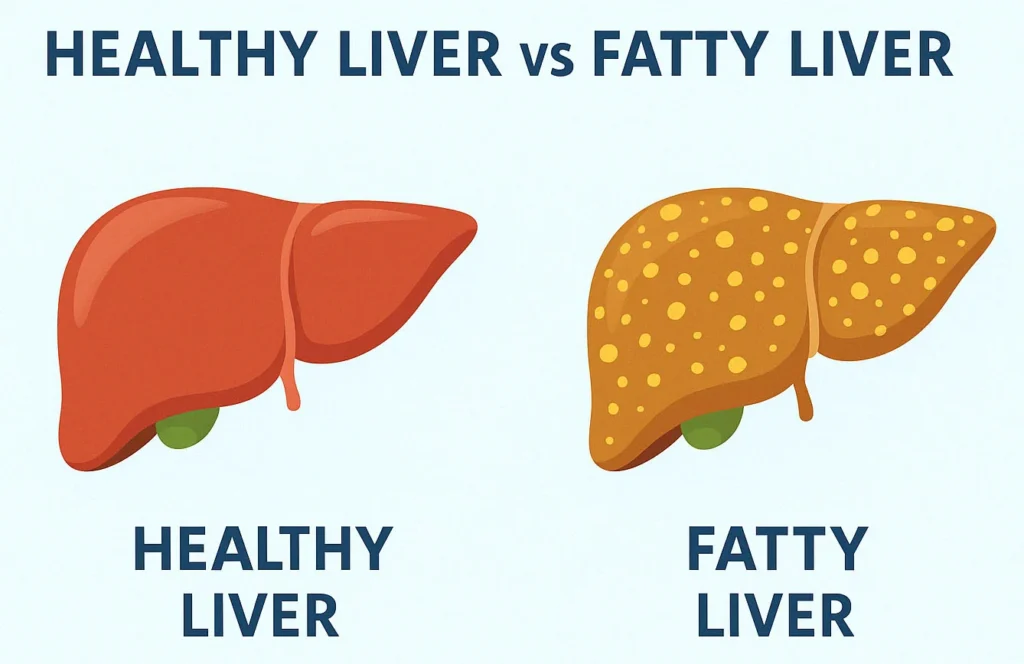
- Simple Steatosis: Fat buildup in liver cells without inflammation or damage.
- Non-Alcoholic Steatohepatitis (NASH): Fat accumulation with inflammation and liver cell injury, which can progress to fibrosis, cirrhosis, or liver cancer.
NAFLD is increasingly being recognized not just as a liver disorder but as part of a broader metabolic syndrome that impacts cardiovascular health, kidney function, and insulin sensitivity.
Causes and Risk Factors
The primary driver of NAFLD is metabolic dysfunction. Key risk factors include:
- Obesity and visceral fat accumulation
- Type 2 diabetes and insulin resistance
- High cholesterol or triglycerides
- Hypertension
- Low physical activity
Even people with normal BMI can develop NAFLD, often called lean NAFLD[2]. Genetic predisposition, gut microbiota imbalances, and rapid weight loss can also contribute to fat accumulation in the liver.
Symptoms and Diagnosis
NAFLD is often called a “silent disease” because it may show no symptoms for years. When symptoms occur, they can include:
- Fatigue
- Discomfort or pain in the upper right abdomen
- Unexplained weight loss
- Enlarged liver on physical exam
Diagnosis is usually done through:
- Blood tests (elevated ALT/AST)
- Liver ultrasound or FibroScan
- FIB-4 or NAFLD fibrosis score
- Occasionally, liver biopsy
Non-invasive scoring systems and imaging tools are increasingly used to stage disease progression without the need for biopsy in many cases.
Potential Complications
If left unmanaged, NAFLD can lead to serious complications:
- Fibrosis: Scar tissue formation in the liver
- Cirrhosis: Advanced liver scarring impairing function
- Hepatocellular carcinoma: Primary liver cancer
- Cardiovascular disease: The leading cause of death in NAFLD patients
- End-stage liver disease: May require liver transplantation

NAFLD vs MASLD
In 2023, international liver associations proposed renaming NAFLD to MASLD (Metabolic dysfunction-Associated Steatotic Liver Disease). The new term aims to better reflect the metabolic nature of the disease[3].
MASLD incorporates steatosis with at least one cardiometabolic risk factor, removing the requirement to exclude alcohol use entirely. This renaming provides a more inclusive, pathophysiology-based approach to diagnosis and classification. It also aligns with a growing trend toward a unified metabolic disease framework that includes diabetes, obesity, and cardiovascular disease.
Treatment and Management
There is no specific FDA-approved medication for NAFLD. Core recommendations include:
- Lose 5–10% of body weight through diet and exercise
- Adopt a Mediterranean or plant-forward diet
- Engage in moderate exercise (e.g. brisk walking) at least 150 minutes per week
- Control comorbidities (blood sugar, blood pressure, lipids)
- Avoid sugar-sweetened beverages and ultra-processed foods
Some medications under investigation include GLP-1 receptor agonists, pioglitazone, and vitamin E, though they are not yet universally recommended without specialist guidance.
Prevention Strategies
Preventing NAFLD relies on early lifestyle interventions:
- Maintain a healthy weight and waist circumference
- Limit saturated fats, added sugars, and refined carbs
- Increase intake of fiber, healthy fats (omega-3), and antioxidants
- Engage in regular aerobic and resistance exercise
- Have regular health checkups to monitor liver enzymes and metabolic parameters
Frequently Asked Questions
Can NAFLD be reversed?
Yes — especially in early stages. Lifestyle changes like weight loss and better diet can reduce liver fat and even reverse inflammation[4].
Is NAFLD the same as fatty liver?
Yes, “fatty liver” is a non-medical term that often refers to NAFLD. However, fatty liver from alcohol is a different condition.
Is NAFLD dangerous?
It can be. While many cases remain stable, others progress to serious liver damage or cardiovascular complications.
What diet is best for NAFLD?
The Mediterranean diet — rich in vegetables, whole grains, olive oil, and lean proteins — is most recommended[5].
What is the difference between NAFLD and MASLD?
MASLD is the updated term for NAFLD that focuses on the presence of metabolic dysfunction, and it broadens the diagnostic criteria to better reflect the disease’s root causes.
References
- NEJM – Epidemiology of NAFLD
- Hepatology – Lean NAFLD
- JHEP Reports – MASLD Nomenclature
- Gastroenterology – Weight Loss and NAFLD
- JHEP – Nutrition and NAFLD
